Post-traumatic stress disorder (PTSD) and substance use disorders (SUD) are, unfortunately, common co-occurrences for veterans, often leading to increased aggression and complicating the healing journey.
Veterans with these dual diagnoses experience complex struggles that impact every facet of life, from personal relationships to community reintegration.
Understanding the biopsychosocial factors at play can illuminate pathways for effective treatment and holistic recovery.
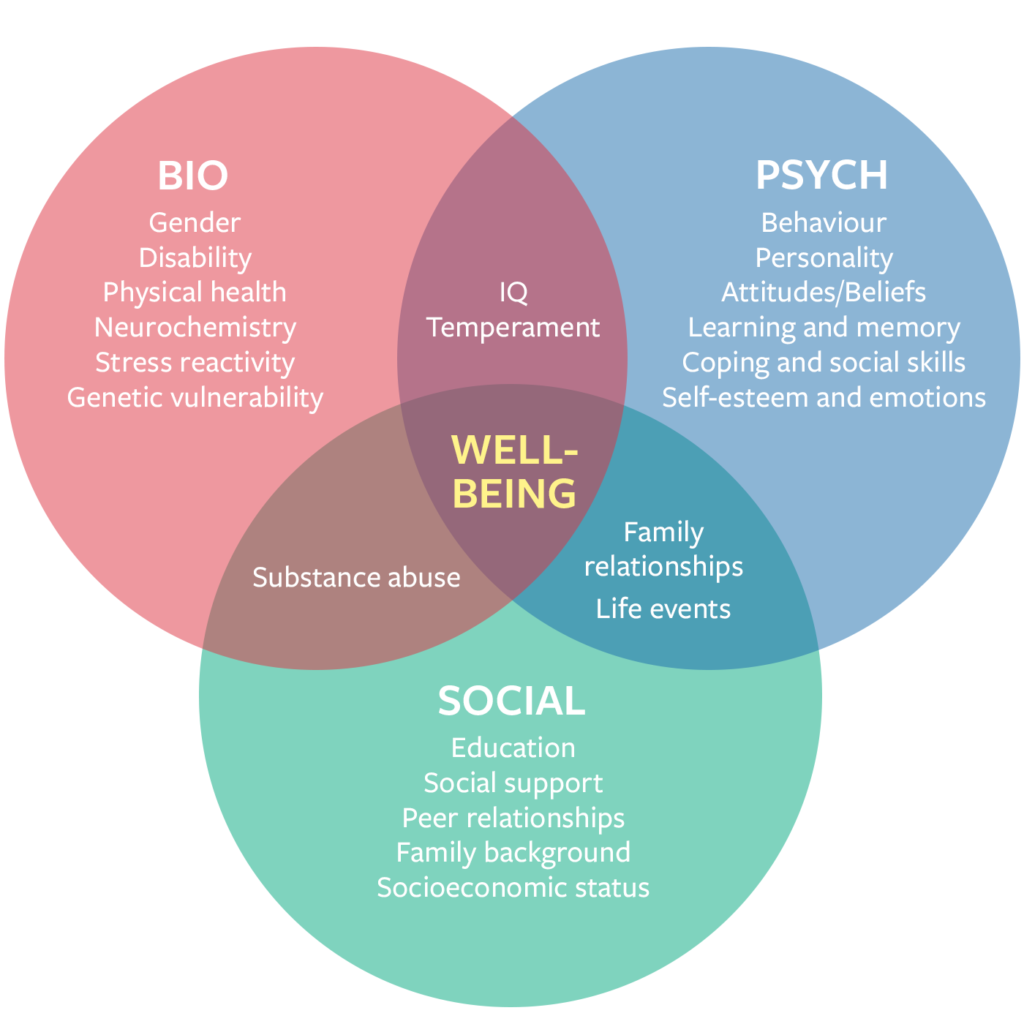
The Biopsychosocial Model
The biopsychosocial model provides a comprehensive approach to understanding the multiple factors influencing aggression among veterans, particularly those with PTSD and SUD.
This model goes beyond symptoms, analyzing biological, psychological, and social factors to provide a well-rounded perspective on veterans’ aggression patterns.
Research reveals that veterans with PTSD and SUD exhibit significantly higher levels of aggression than veterans without these conditions. Substance use, trauma-related emotional dysregulation, and peer influence all contribute to this aggression and make it difficult for veterans to maintain stable relationships and find a sense of peace (Heinz et al., 2014; Veterans With Recent Substance Use and Aggression, 2019).
For veterans dealing with trauma, PTSD often manifests in re-experiencing symptoms, heightened vigilance, and emotional numbness, which can drive aggressive behaviors. When combined with substance use, these factors can become even more explosive, often leading veterans into risky situations or deepening interpersonal conflicts.
Through biopsychosocial analysis, we can see how emotional triggers, impulsivity, and social environments interact to worsen aggressive tendencies.
The Impact of Trauma on the Brain
The biological component of the biopsychosocial model sheds light on how trauma impacts brain structure and chemistry.
Chronic stress from trauma leads to the over activation of the amygdala, the brain’s fear center, while diminishing the functionality of the prefrontal cortex, which regulates decision-making and impulse control. This imbalance contributes to heightened states of aggression and impulsive reactions in veterans.
Additionally, studies have shown that prolonged exposure to stress alters neurotransmitters like serotonin and dopamine, affecting mood regulation and leading some veterans toward substance use as a form of self-medication.
Valor Therapeutics incorporates knowledge of these biological impacts in its treatment plans by offering therapy that helps veterans regain control over their responses.
Techniques like biofeedback and mindfulness training are used to retrain the brain, reducing hyper arousal and helping veterans achieve a sense of calm.
Cognitive-behavioral therapy (CBT) also plays a critical role by reshaping thought patterns that trigger aggressive reactions, empowering veterans to manage their behaviors more effectively.
Emotional Dysregulation and Coping Mechanisms
The psychological aspects of PTSD and SUD encompass a veteran’s internal struggles with emotional regulation, trauma, and self-worth.
Veterans often experience overwhelming feelings of guilt, shame, or anger related to their service experiences, which can fuel both substance use and aggression. In the absence of effective coping mechanisms, veterans may resort to alcohol or drugs to numb these intense emotions.
Unfortunately, this often results in a cycle where substance use exacerbates aggressive behavior, further isolating veterans from supportive relationships.
Valor Therapeutics addresses these psychological factors through individualized therapy plans that include exposure therapy and trauma-focused CBT. These therapies allow veterans to confront and process traumatic memories in a controlled environment, reducing the power these memories hold over their emotional responses.
Valor also provides training in emotional regulation techniques, such as deep breathing, grounding exercises, and visualization, to help veterans manage their impulses and build resilience. By enhancing emotional self-awareness and control, Valor supports veterans in developing healthier coping strategies that replace substance use and aggressive outbursts.
The Role of Social Networks and Peer Influence
Social networks play a significant role in either amplifying or mitigating aggression in veterans with PTSD and SUD.
Veterans with close friends or family who frequently engage in substance use or exhibit aggressive behavior are more likely to reflect these behaviors in their own lives.
The research shows that social networks characterized by substance use and aggression can increase the likelihood of similar behaviors in veterans( (Veterans With Recent Substance Use and Aggression, 2019).
Given this dynamic, it’s crucial to address these social influences within therapeutic settings. Valor Therapeutics focuses on creating healthy, supportive communities for veterans, ensuring they have positive role models and supportive peers during treatment.
This approach not only helps veterans form healthier relationships but also reduces the risk of aggressive incidents.
A Path Toward Holistic Healing
At Valor Therapeutics, we focus on integrative, trauma-informed methods that address veterans’ needs holistically, acknowledging the biological, psychological, and social facets of healing.
Here’s how we support veterans:
- Individualized Therapy: Veterans receive customized treatment plans that incorporate evidence-based practices, such as trauma-focused therapy and alternative treatments. These personalized approaches ensure therapy adapts to each veteran’s unique needs and background.
- Community and Peer Support: Recognizing the strength of communal bonds, Valor fosters peer support networks and group therapy. This community-centered approach builds mutual trust, accountability, and the social bonds essential for recovery.
- Skill-Building for Resilience: Veterans are empowered with mindfulness, stress management, and emotional regulation skills to cope with challenges. Valor’s holistic approach supports veterans in managing daily stressors and maintaining emotional stability in diverse situations.
- Family Integration: We offer resources and family education sessions, allowing loved ones to understand PTSD and SUD and providing veterans with a network of support that reinforces healing.
- Long-Term Support and Reintegration: Valor provides aftercare and ongoing resources to ensure veterans transition smoothly back into civilian life. Our reintegration support gives veterans the tools to thrive, both within and beyond treatment.
Why a Biopsychosocial Approach Matters
The biopsychosocial approach to healing recognizes that veterans are complex individuals whose struggles cannot be addressed by a one-size-fits-all solution.
By considering biological, psychological, and social dimensions, Valor Therapeutics provides a holistic treatment framework that supports veterans in reclaiming their lives. This approach is essential because it addresses the root causes of PTSD, SUD, and aggression, rather than merely managing symptoms.
Through Valor’s comprehensive, biopsychosocial approach, veterans are empowered to rebuild their lives, form meaningful relationships, and find peace within themselves.
For these individuals, healing is not just about recovery; it’s about rediscovering self-worth, developing resilience, and embracing a future full of possibility.
References
Heinz, A. J., Makin-Byrd, K., Blonigen, D. M., Reilly, P., & Timko, C. (2014). Aggressive behavior among military veterans in substance use disorder treatment: The roles of posttraumatic stress and impulsivity. *Addictive Behaviors*, *39*(3), 536–543. https://doi.org/10.1016/j.addbeh.2013.10.016
Veterans With Recent Substance Use and Aggression: PTSD, Substance Use, and Social Network Behaviors. (2019). *Psychological Trauma: Theory, Research, Practice, and Policy, 11*(4), 424–433. https://doi.org/10.1037/tra0000367

Melissa Henderson
Melissa Henderson is a dual-major student in Organizational Leadership and Psychology at Wright State University. With experience in nonprofit support and advocacy for veterans, she’s dedicated to creating positive, inclusive environments that empower individuals and promote well-being. Driven by her values of resilience and collaboration, Melissa is committed to leadership that makes a lasting impact on both people and systems.